How to Speed Up Muscle Strain Recovery in Athletes

How to Speed Up Muscle Strain Recovery in Athletes Muscle injuries are one of the most common problems athletes face. Whether you are a professional player or a fitness enthusiast, a muscle strain can interrupt training, reduce performance, and delay competition plans. Many athletes search for how to speed up muscle strain recovery because they want to return to sports safely and quickly. The truth is, recovery cannot be rushed artificially, but it can be optimized with the right approach. This guide explains the healing process, recovery stages, rehabilitation principles, and safe return-to-play strategies in a structured and easy-to-understand format. Understanding Muscle Strain in Athletes A muscle strain occurs when muscle fibers are overstretched or torn due to sudden force or excessive load. This commonly happens during sprinting, jumping, rapid direction changes, or heavy lifting. Muscle strains are classified into three grades. Mild strains involve microscopic damage and cause slight discomfort. Moderate strains include partial tears and noticeable weakness. Severe strains involve complete tears and significant loss of muscle function. Athletes frequently experience strains in the hamstrings, quadriceps, calves, and lower back. A muscle strain in back often develops due to improper lifting mechanics or weak core stability. Similarly, an abdominal muscle strain is common in sports that involve twisting movements, such as cricket, tennis, and throwing events. Understanding the severity of injury is the first step toward knowing how to heal muscle strain effectively. The Healing Process: What Happens Inside the Muscle To understand how to speed up muscle strain recovery, it is important to know how muscles heal. Muscle healing occurs in three main phases: 1. Inflammatory Phase (First 72 Hours) The body sends blood and immune cells to the injured area. Swelling and pain are common during this stage. This is a protective response. 2. Repair Phase (3 Days to 3 Weeks) New muscle fibers begin forming. Collagen develops to rebuild damaged tissue. 3. Remodeling Phase (3 Weeks and Beyond) The new tissue becomes stronger and more organized. Gradual strengthening is essential during this phase. If rehabilitation is not structured properly, scar tissue may form incorrectly, increasing the risk of re-injury. Early Management: The First 72 Hours Matter The initial phase determines how quickly and safely recovery progresses. During the first 48–72 hours, the goal is to control inflammation. Rest is important, but complete immobility should be avoided unless the injury is severe. Ice application for short intervals helps reduce swelling and pain. Compression and elevation may further assist in controlling inflammation. This early care forms the foundation of how to treat muscle strain safely and effectively. When and How to Start Movement Many athletes make the mistake of either returning too early or resting for too long. Both can delay healing. After the initial inflammatory phase, gentle, pain-free movement should begin. Controlled activation improves blood circulation and supports proper alignment of healing fibers. Light stretching without pain, simple mobility exercises, and isometric contractions can help restore muscle function. For example, in a muscle strain in back, controlled core activation and posture correction exercises support recovery. In an abdominal muscle strain, breathing exercises and gentle trunk stabilization are helpful during early stages. This balanced approach is essential for those wondering how to cure muscle strain efficiently. Strengthening Phase: Building Back Muscle Capacity Once pain reduces and movement improves, strengthening becomes critical. Muscles heal stronger when gradually exposed to controlled resistance. At this stage, light resistance exercises, band training, and progressive loading are introduced. Eccentric strengthening is particularly beneficial because it improves muscle control and resilience. Athletes must avoid aggressive stretching or heavy loading too soon. Progressive strengthening ensures safe tissue remodeling and reduces recurrence risk. If someone asks how to heal muscle strain completely, the answer always includes structured strengthening, not just rest. The Role of Nutrition in Faster Recovery Nutrition plays a significant role in muscle repair. Protein supports muscle fiber regeneration. Athletes recovering from a muscle strain should ensure adequate daily protein intake from balanced sources. Hydration is equally important because fluid balance supports circulation and cellular repair. Anti-inflammatory nutrients such as omega-3 fatty acids, leafy vegetables, and antioxidant-rich foods can support the healing process. However, nutrition works best when combined with proper rehabilitation. Sleep and Hormonal Recovery Sleep is often underestimated in injury recovery. During deep sleep, growth hormone secretion increases, accelerating tissue repair. Athletes should prioritize 7–9 hours of quality sleep during the healing period. Without proper rest, even the best rehabilitation program may not deliver optimal results. Special Considerations for Back and Abdominal Strains A muscle strain in back requires attention to posture, hip mobility, and core strength. Weak supporting muscles can overload the lower back, delaying recovery. An abdominal muscle strain requires gradual progression in rotational movements. Sudden twisting or aggressive core workouts too early can worsen the injury. These specific adjustments are essential when considering how to speed up muscle strain recovery in athletes participating in rotational or lifting sports. Safe Return to Sports Returning too early is one of the most common reasons for re-injury. Before returning to full training, the athlete should have: Full pain-free range of motion Nearly equal strength compared to the uninjured side Ability to perform sport-specific drills without discomfort No swelling after practice sessions Gradual return-to-play progression ensures long-term success. Common Mistakes That Delay Recovery Many athletes unknowingly slow down recovery by: Ignoring mild pain Skipping rehabilitation exercises Returning to competition too soon Not correcting training errors Overstretching in the early stages Understanding these mistakes is part of knowing how to treat muscle strain correctly. Realistic Recovery Timeline Recovery depends on severity. Mild strains may heal within one to two weeks. Moderate injuries typically require three to six weeks. Severe tears may take several months and sometimes need medical supervision. Patience combined with structured rehabilitation is the safest path forward. FAQs How long does a muscle strain usually take to heal? Mild strains heal within 1–2 weeks, moderate injuries may take 3–6 weeks, and severe tears can require several months. What is
Shoulder Bone Fracture Treatment: Symptoms and Care
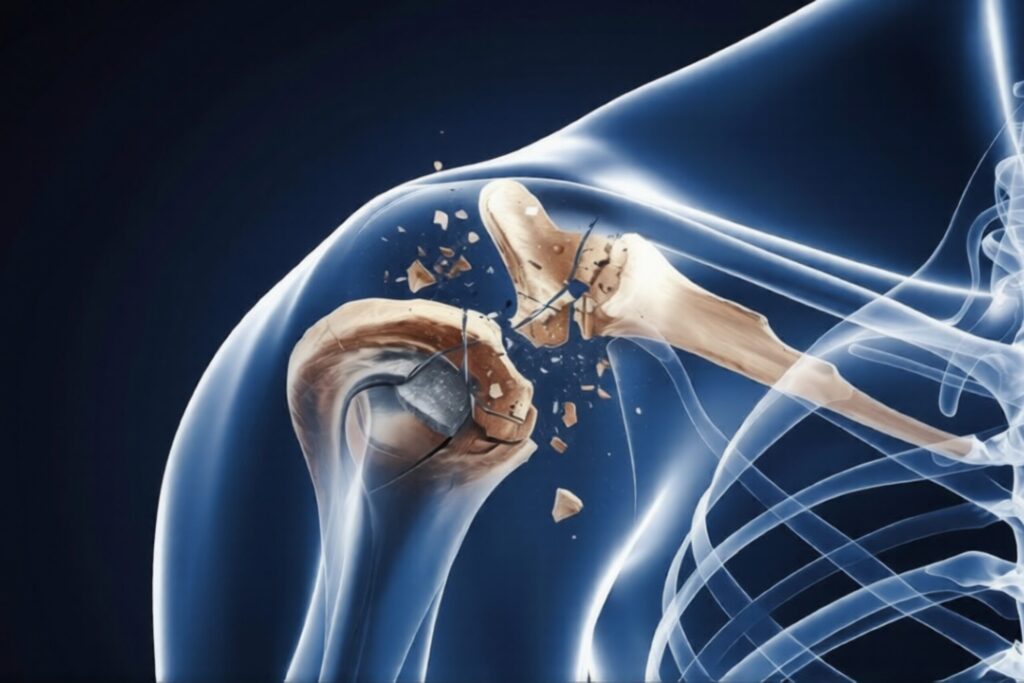
Shoulder Bone Fracture Treatment: Symptoms and Care A shoulder injury can be painful and frightening, especially when it involves a broken bone. Understanding shoulder bone fracture treatment is important so that patients receive timely care, avoid complications, and return to normal activities safely. The shoulder is a complex joint made up of bones, ligaments, tendons, and muscles. When any part of this structure is damaged, movement and daily function can be affected. In this detailed guide, you will learn about symptoms, causes, diagnosis, treatment options, recovery process, and related conditions such as shoulder ligament injuries and frozen shoulder. The goal is to provide clear, easy-to-understand, and medically accurate information. What Is a Shoulder Bone Fracture? A shoulder bone fracture occurs when one of the bones in the shoulder region breaks due to trauma or excessive force. The shoulder consists of three main bones: Clavicle (collarbone) Scapula (shoulder blade) Proximal humerus (upper arm bone) A fracture can occur in any of these bones, but clavicle and proximal humerus fractures are most common. Immediate shoulder bone fracture treatment is necessary to reduce pain, ensure proper bone alignment, and prevent long-term stiffness or deformity. Common Causes of Shoulder Bone Fracture Understanding the cause helps doctors decide the right shoulder fracture treatment plan. 1. Road Traffic Accidents High-impact injuries from bike or car accidents are a major cause. 2. Sports Injuries Falls during cricket, football, kabaddi, or gym workouts may lead to fractures. 3. Fall on an Outstretched Arm This is common in elderly patients. 4. Osteoporosis Weak bones increase fracture risk, especially in older adults. Early diagnosis ensures proper shoulder bone fracture treatment and faster healing. Symptoms of Shoulder Bone Fracture Recognizing symptoms quickly helps prevent complications. Severe Shoulder Pain Intense shoulder pain immediately after injury. Swelling and Bruising Visible swelling around the shoulder joint. Limited Movement Difficulty lifting the arm. Deformity In some cases, the shoulder may look uneven or displaced. If you experience these symptoms, seek immediate medical care. Diagnosis of Shoulder Bone Fracture Doctors use the following methods: Physical Examination Checking swelling, tenderness, and movement restriction. X-Ray Confirms the location and severity of the fracture. CT Scan Used in complex fractures for surgical planning. Proper diagnosis guides the correct shoulder bone fracture treatment strategy. Types of Shoulder Bone Fractures Treatment depends on fracture type. Non-Displaced Fracture Bone remains aligned. Usually shown to be stable on X-ray. Displaced Fracture Bone fragments are separated. Comminuted Fracture The bone breaks into multiple pieces. Each type requires a different shoulder fracture treatment approach. Shoulder Bone Fracture Treatment Options The method of shoulder bone fracture treatment depends on severity, patient age, and activity level. Non-Surgical Shoulder Bone Fracture Treatment Many shoulder fractures heal without surgery. Sling Immobilization Arm is supported in a sling for 3–6 weeks. Pain Management Medications to control shoulder pain. Physiotherapy Gentle exercises after initial healing to prevent stiffness. Non-surgical treatment is common in minor fractures and elderly patients. Surgical Shoulder Bone Fracture Treatment Surgery may be required when: Bones are severely displaced Fracture involves joint surface Multiple bone fragments exist Surgical Methods Plate and screw fixation Rod fixation Shoulder replacement (in severe cases) Surgery ensures stable bone healing and better long-term function. Recovery Timeline After Shoulder Bone Fracture Healing usually takes 6 to 12 weeks, depending on severity. First 2 Weeks Pain and swelling control. 3–6 Weeks Gradual arm movement exercises. 6–12 Weeks Strength training and physiotherapy. Following the correct shoulder bone fracture treatment plan improves outcomes. Shoulder Fracture Treatment vs Shoulder Ligament Tear Treatment Sometimes a fracture is accompanied by soft tissue damage. Shoulder Fracture Treatment Bone break due to fall or trauma Managed with sling, medicines, or surgery Focus on proper bone healing Shoulder Ligament Tear Treatment Ligament injury affects joint stability Treated with rest and physiotherapy Severe cases may need arthroscopic repair Both conditions require accurate diagnosis for complete shoulder recovery. Frozen Shoulder After Fracture Some patients develop stiffness after injury or surgery. What Is Frozen Shoulder? Frozen shoulder causes pain and restricted movement. Frozen Shoulder Treatment Options Physiotherapy Anti-inflammatory medications Joint injections In rare cases, arthroscopic release Early rehabilitation reduces the risk of needing best treatment for frozen shoulder later. Managing Shoulder Pain During Recovery Persistent shoulder pain can delay healing. Tips: Follow doctor’s instructions Avoid heavy lifting Attend regular physiotherapy Use ice packs as advised Pain gradually decreases as healing progresses. Complications If Not Treated Properly Ignoring or delaying shoulder bone fracture treatment may lead to: Permanent stiffness Malunion (improper bone healing) Chronic shoulder pain Joint arthritis Muscle weakness Timely care prevents these issues. Prevention Tips for Shoulder Injuries Wear protective sports gear Maintain bone strength with calcium Improve balance to prevent falls Strengthen shoulder muscles Prevention is always better than long-term treatment. When to See an Orthopedic Specialist Consult a specialist if: Pain is severe Movement is limited Swelling increases Deformity is visible Early orthopedic evaluation ensures correct shoulder fracture treatment and better recovery. FAQs How long does shoulder bone fracture treatment take? Healing usually takes 6–12 weeks, but full recovery may take 3–4 months with physiotherapy. Can shoulder fractures heal without surgery? Yes, many fractures heal with sling support and physiotherapy. What is the best treatment for frozen shoulder after fracture? The best treatment for frozen shoulder includes physiotherapy, medication, and sometimes joint injections. Is shoulder pain normal after fracture healing? Mild discomfort is normal during recovery, but severe or persistent pain should be evaluated. What is the difference between shoulder ligament tear treatment and fracture treatment? Fracture treatment focuses on bone healing, while shoulder ligament tear treatment repairs soft tissue structures. Conclusion A shoulder injury should never be ignored. Proper shoulder bone fracture treatment ensures correct healing, reduces pain, and restores full movement. Early diagnosis, structured rehabilitation, and expert orthopedic care are key to successful recovery. Understanding symptoms, following medical advice, and completing physiotherapy are essential steps toward regaining shoulder strength and function. If you experience persistent shoulder pain or limited movement after injury, seek medical evaluation immediately.
ACL Surgery Cost in India for Sports Injury Treatment

ACL Surgery Cost in India for Sports Injury Treatment Sports injuries are increasingly common among professional athletes, fitness enthusiasts, and even recreational players. One of the most serious knee injuries is an ACL tear. If you or someone in your family has been advised surgery, the first question that usually comes to mind is about ACL surgery cost. This detailed guide explains ACL surgery pricing in India, treatment options, recovery expectations, and important medical considerations. The objective is to provide clarity so patients can make informed healthcare decisions. Understanding ACL Injury and Why Surgery Is Needed The Anterior Cruciate Ligament (ACL) is one of the key stabilizing ligaments in the knee joint. It connects the femur (thigh bone) to the tibia (shin bone) and prevents excessive forward movement and rotation. An ACL tear commonly occurs during: Football Cricket Basketball Kabaddi Sudden twisting injuries Road accidents A complete ACL tear often requires ACL surgery because the ligament does not heal naturally. Without surgical reconstruction, patients may experience instability, repeated knee giving-way episodes, and long-term cartilage damage. ACL Surgery Cost in India – Complete Breakdown When discussing ACL surgery cost, it is important to understand that pricing varies based on hospital type, city, surgeon expertise, implant quality, and rehabilitation services. Average ACL Surgery Cost in India In India, the ACL surgery cost typically ranges between: ₹1,20,000 to ₹3,50,000 in private hospitals ₹60,000 to ₹1,20,000 in government hospitals Metro cities like Delhi NCR, Mumbai, and Bangalore generally have slightly higher costs due to infrastructure and specialist availability. Factors That Affect ACL Surgery Cost Several medical and non-medical factors influence ACL surgery cost: Hospital Category – NABH-accredited hospitals may charge more. Surgeon’s Expertise – Experienced arthroscopic surgeons may have higher fees. Implant Type – Bio-absorbable screws, titanium implants, or imported graft fixation systems can increase cost. Room Category – General ward vs private or deluxe rooms. Additional Injuries – Meniscus repair or cartilage procedures increase expense. Rehabilitation Cost – Physiotherapy sessions after surgery.Understanding these components helps patients estimate the total financial commitment. Types of ACL Surgery and Their Cost Impact The types of ACL surgery also influence pricing and recovery. Arthroscopic ACL Reconstruction This is the most common method. It is minimally invasive and performed using a camera (arthroscope). Faster recovery Smaller incisions Reduced hospital stay Most modern ACL surgery cost calculations are based on arthroscopic techniques. Autograft vs Allograft Surgery Autograft Surgery – Uses the patient’s own tendon (hamstring or patellar tendon). Allograft Surgery – Uses donor tissue. Autografts are more common in India and relatively cost-effective. Allografts may increase ACL surgery cost due to graft procurement charges. Detailed Expense Structure of ACL Surgery To understand ACL surgery cost clearly, here is a breakdown: 1. Pre-Surgery Expenses MRI scan Blood tests Orthopedic consultation 2. Surgical Charges Operation theatre charges Surgeon fees Anesthesia charges 3. Implant & Graft Cost This is one of the biggest components affecting ACL surgery cost. 4. Hospital Stay Usually 1–3 days. 5. Post-Surgery Physiotherapy Rehabilitation is crucial for full knee recovery. ACL Surgery Recovery Time – What to Expect A common concern apart from ACL surgery cost is ACL surgery recovery time. Recovery typically progresses in stages: First 2 Weeks Swelling reduction Pain management Gentle range-of-motion exercises 1 to 3 Months Strength-building exercises Partial return to normal walking 4 to 6 Months Light jogging Agility training 6 to 9 Months Return to sports (depending on rehabilitation progress) Athletes may require structured physiotherapy programs to ensure safe return to play. ACL Tear Surgery Procedure Explained During ACL tear surgery, the torn ligament is removed and replaced with a graft. The surgeon drills small tunnels in the tibia and femur to fix the new ligament securely. The surgery usually takes 60–90 minutes and is done under spinal or general anesthesia. Most patients are discharged within 24–48 hours. Bad Signs After ACL Surgery – When to Consult a Doctor While ACL surgery is generally safe, patients should be aware of potential complications. Warning Signs Include: Persistent high fever Excessive swelling Redness or discharge from incision Severe calf pain Limited knee movement beyond expected levels Recognizing these bad signs after ACL surgery early can prevent serious complications. Is ACL Surgery Covered by Insurance? Many health insurance policies in India cover ACL surgery cost under hospitalization benefits. However: Waiting period may apply Pre-existing injury clauses may affect coverage Sub-limits on implants may exist Patients should check policy terms before admission. Why Timely ACL Surgery Is Important for Athletes Ignoring ACL injury can lead to: Repeated knee instability Meniscus damage Early osteoarthritis Reduced sports performance For athletes and active individuals, early intervention reduces long-term damage and improves functional outcomes. How to Reduce ACL Surgery Cost Patients can manage ACL surgery cost by: Comparing hospital packages Choosing in-network insurance hospitals Opting for standard room categories Confirming implant pricing in advance Checking cashless insurance options Transparent financial planning prevents unexpected expenses. Long-Term Outcome After ACL Surgery Most patients regain normal knee function with proper rehabilitation. Success rates are high when surgery is performed by experienced orthopedic surgeons. Key to success: Structured physiotherapy Muscle strengthening Avoiding premature sports return Regular follow-ups FAQs What is the average ACL surgery cost in India? The ACL surgery cost in India ranges between ₹1,20,000 and ₹3,50,000 in private hospitals depending on surgeon, hospital, and implant type. What is ACL surgery recovery time? ACL surgery recovery time typically ranges from 6 to 9 months for full return to sports activities. What are the types of ACL surgery? The main types of ACL surgery include arthroscopic ACL reconstruction, autograft reconstruction, and allograft reconstruction. How long does ACL tear surgery take? ACL tear surgery generally takes 60 to 90 minutes, and patients are discharged within 1–2 days. What are bad signs after ACL surgery? Bad signs after ACL surgery include fever, excessive swelling, redness, wound discharge, severe pain, and restricted knee movement. Conclusion Understanding ACL surgery cost in India for sports injury treatment is essential for financial planning and informed decision-making.
ACL Reconstruction सर्जरी के बाद कितने समय में सामान्य चलना और खेलना संभव है?

ACL Reconstruction सर्जरी के बाद कितने समय में सामान्य चलना और खेलना संभव है? ACL Reconstruction Surgery घुटने की एक महत्वपूर्ण शल्य प्रक्रिया है, जो तब की जाती है जब ACL लिगामेंट पूरी तरह या गंभीर रूप से फट जाता है। ACL घुटने के चार प्रमुख लिगामेंट्स में से एक है, जो घुटने को स्थिरता प्रदान करता है और आगे-पीछे तथा घुमावदार गति को नियंत्रित करता है। खेल के दौरान अचानक मुड़ना, गलत तरीके से उतरना, सड़क दुर्घटना या तेज झटका लगने से ACL चोट हो सकती है। ऐसे में अक्सर मरीज का सबसे बड़ा प्रश्न होता है — ACL Reconstruction सर्जरी के बाद सामान्य चलना और खेलना कब संभव होगा? इस लेख में हम ACL सर्जरी रिकवरी समय, ACL टियर सर्जरी, ACL सर्जरी के प्रकार, ACL सर्जरी के बाद खराब संकेत और संपूर्ण पुनर्वास प्रक्रिया को विस्तार से समझेंगे। ACL लिगामेंट क्या है और इसकी भूमिका क्यों महत्वपूर्ण है? ACL (Anterior Cruciate Ligament) जांघ की हड्डी और पिंडली की हड्डी को जोड़ने वाला प्रमुख लिगामेंट है। यह घुटने को स्थिरता देता है, आगे खिसकने से रोकता है और अचानक मुड़ने या दिशा बदलने के दौरान संतुलन बनाए रखता है, जिससे चलना, दौड़ना और कूदना सुरक्षित रहता है। घुटने को आगे की ओर खिसकने से रोकना घुटने की घुमावदार स्थिरता बनाए रखना अचानक दिशा बदलते समय संतुलन देना यदि यह लिगामेंट फट जाए, तो घुटना अस्थिर महसूस होता है, बार-बार मुड़ सकता है और सामान्य चलना भी कठिन हो जाता है। ACL टियर सर्जरी कब आवश्यक होती है? जब ACL पूरी तरह फट जाता है, तो घुटने में अस्थिरता, अचानक मुड़ जाना, सूजन, दर्द और चलने-दौड़ने में कठिनाई जैसी समस्याएँ दिखाई देती हैं। ऐसे मामलों में घुटना सामान्य गतिविधियों के दौरान भी साथ नहीं देता और बार-बार लड़खड़ाने का अनुभव होता है, तब शल्य उपचार की आवश्यकता पड़ सकती है। चलते समय घुटना मुड़ जाना बार-बार सूजन आना खेल या दौड़ने में असमर्थता एमआरआई में पूर्ण टियर दिखाई देना तब डॉक्टर ACL टियर सर्जरी की सलाह देते हैं। यह सर्जरी घुटने की स्थिरता बहाल करने के लिए की जाती है। ACL सर्जरी के प्रकार ACL सर्जरी के प्रकार मुख्यतः उपयोग किए गए ग्राफ्ट पर आधारित होते हैं। 1. स्वयं के शरीर से ग्राफ्ट (ऑटोग्राफ्ट तकनीक) इसमें मरीज के हैमस्ट्रिंग या पाटेला टेंडन का उपयोग किया जाता है। यह सबसे अधिक प्रचलित और सुरक्षित तरीका माना जाता है। 2. डोनर ग्राफ्ट (एलोग्राफ्ट तकनीक) इसमें किसी डोनर से प्राप्त टेंडन का उपयोग किया जाता है। यह उन मरीजों के लिए उपयुक्त है जिन्हें कम आक्रामक प्रक्रिया चाहिए। 3. आधुनिक आर्थ्रोस्कोपिक तकनीक आज अधिकांश ACL Reconstruction Surgery आर्थ्रोस्कोपी द्वारा की जाती है, जिसमें छोटे चीरे लगाए जाते हैं और रिकवरी तेज होती है। ACL सर्जरी रिकवरी समय ACL सर्जरी के बाद ठीक होने का समय मरीज की उम्र, शारीरिक स्थिति, अपनाई गई शल्य तकनीक और पुनर्वास कार्यक्रम पर निर्भर करता है। सामान्यतः रिकवरी को अलग-अलग चरणों में बाँटा जाता है। पहला चरण (0–2 सप्ताह) सूजन और दर्द नियंत्रण घुटने को सीधा रखने के व्यायाम बैसाखी की सहायता से चलना हल्की फिजियोथेरेपी शुरू दूसरा चरण (3–6 सप्ताह) बिना सहारे धीरे-धीरे चलना मांसपेशियों को मजबूत बनाना घुटने को 120 डिग्री तक मोड़ना तीसरा चरण (2–4 महीने) संतुलन और स्थिरता व्यायाम हल्की जॉगिंग सीढ़ियाँ सामान्य रूप से चढ़ना चौथा चरण (5–9 महीने) खेल संबंधित अभ्यास दिशा बदलने वाले व्यायाम पूर्ण खेल गतिविधि की तैयारी अधिकांश मरीजों में 6 से 9 महीने में खेल में वापसी संभव होती है। ACL सर्जरी के बाद सामान्य चलना कब संभव है? 1–2 सप्ताह में सहारे से चलना 4–6 सप्ताह में सामान्य चलना 3 महीने में बिना दर्द और आत्मविश्वास के साथ चलना ACL सर्जरी के बाद खेल कब शुरू करें? घुटने में सूजन न हो मांसपेशियों की ताकत 90% तक वापस आ जाए संतुलन परीक्षण पास हो डॉक्टर और फिजियोथेरेपिस्ट की अनुमति आमतौर पर 6–9 महीने बाद प्रतिस्पर्धात्मक खेल संभव होता है, लेकिन यह पूरी तरह मरीज की रिकवरी, मांसपेशियों की ताकत, संतुलन और डॉक्टर की अनुमति पर निर्भर करता है। यदि फिजियोथेरेपी सही तरीके से पूरी की गई हो और घुटने में कोई सूजन या दर्द न हो, तभी सुरक्षित रूप से खेल में वापसी करनी चाहिए, ताकि दोबारा चोट लगने का खतरा कम हो सके। ACL सर्जरी के बाद खराब संकेत लगातार बढ़ती सूजन तेज दर्द जो कम न हो घाव से पस निकलना बुखार घुटने में असामान्य ढीलापन ये ACL सर्जरी के बाद दिखाई देने वाले गंभीर और चिंताजनक संकेत हो सकते हैं, इसलिए ऐसी स्थिति में तुरंत किसी विशेषज्ञ डॉक्टर से चिकित्सकीय सलाह लेना बेहद आवश्यक होता है। क्या बिना सर्जरी ACL ठीक हो सकता है? आंशिक टियर में कुछ मामलों में बिना सर्जरी उपचार संभव है, लेकिन पूर्ण टियर में ACL Reconstruction Surgery ही स्थायी समाधान मानी जाती है। FAQ (अक्सर पूछे जाने वाले प्रश्न) एसीएल सर्जरी के बाद पूरी तरह ठीक होने में कितना समय लगता है? सामान्यतः 6–9 महीने, लेकिन यह व्यक्ति की शारीरिक स्थिति और व्यायाम अनुशासन पर निर्भर करता है। क्या एसीएल सर्जरी के बाद दोबारा चोट लग सकती है? हाँ, यदि पुनर्वास अधूरा हो या जल्दबाजी में खेल शुरू किया जाए। क्या एसीएल सर्जरी के बाद दौड़ना सुरक्षित है? डॉक्टर की अनुमति के बाद 3–4 महीने में हल्की दौड़ शुरू की जा सकती है। एसीएल सर्जरी के बाद खराब संकेत कौन से हैं? लगातार सूजन, तेज दर्द, संक्रमण और घुटने की अस्थिरता। क्या सभी एसीएल टियर में सर्जरी जरूरी होती है? नहीं, आंशिक टियर में कुछ मामलों में बिना सर्जरी उपचार संभव है। निष्कर्ष ACL Reconstruction Surgery के बाद सामान्य चलना लगभग 4–6 सप्ताह में संभव हो सकता है, जबकि खेल गतिविधियों में पूरी तरह वापसी के लिए 6–9 महीने का समय लग सकता है। सही समय पर ACL टियर सर्जरी, उचित ACL सर्जरी तकनीक का चयन, और अनुशासित पुनर्वास कार्यक्रम ही सफल परिणाम की कुंजी हैं। यदि आप सुरक्षित और सफल ACL सर्जरी करवाना चाहते हैं, तो Dr. Himanshu Gupta एक अनुभवी और कुशल ऑर्थोपेडिक सर्जन हैं, जिन्हें ACL Reconstruction Surgery और स्पोर्ट्स इंजरी उपचार में विशेष विशेषज्ञता प्राप्त है। उनकी उन्नत आर्थ्रोस्कोपिक तकनीक और संरचित पुनर्वास मार्गदर्शन मरीजों को तेज, सुरक्षित और स्थायी रिकवरी में मदद करता
Partial ACL Tear: Symptoms, Causes, Treatment & Recovery Guide

Partial ACL Tear: Symptoms, Causes, Treatment & Recovery Guide A partial ACL tear is a common knee ligament injury in which the anterior cruciate ligament is damaged but not completely ruptured. The ACL plays an essential role in stabilizing the knee joint, supporting movement, and preventing excessive forward motion of the shin bone. When some fibers of the ligament are injured, patients may still be able to walk but often experience pain, instability, and reduced performance during physical activity. People searching for information about partial ACL tear symptoms, treatment, MRI diagnosis, and partial ACL tear recovery time without surgery usually want clear guidance on healing options and long-term outcomes. Understanding whether do partial ACL tears heal, how rehabilitation works, and when to use a knee brace for ACL tear helps patients make informed treatment decisions. This comprehensive guide explains what a partial ACL tear is, its symptoms, MRI diagnosis, treatment options, recovery process, long-term effects without surgery, and answers common patient questions in a simple and human-friendly way. What Is a Partial ACL Tear? A partial ACL tear is a condition in which the anterior cruciate ligament is only partially torn, allowing the knee to retain some stability. Despite limited fiber damage, patients may experience pain, swelling, and functional difficulty, especially during twisting movements or sports. Key Features of Partial ACL Tear Partial loss of knee stability: The knee may feel weak, especially during sudden pivoting or turning motions. Swelling and tenderness: Inflammation develops around the joint, causing discomfort and limited movement. Pain during activity: Walking, running, or climbing stairs may trigger moderate knee pain. Reduced range of motion: Bending and straightening the knee can be stiff and limited. Partial ACL tears require proper assessment to restore knee function and prevent long-term instability or secondary injuries. Symptoms of Partial ACL Tear Symptoms of a partial ACL tear may be subtle initially but tend to worsen with physical activity. Early identification of signs can improve recovery outcomes and prevent further knee damage. Common Symptoms Include Knee pain during activity: Moderate discomfort often increases when twisting or landing from jumps. Swelling within 24 hours: The knee may swell due to internal bleeding or fluid accumulation. Feeling of instability: The joint may “give way” unexpectedly during walking or running. Difficulty performing movements: Daily activities like climbing stairs or squatting can be challenging. Recognizing these symptoms early supports effective rehabilitation and minimizes long-term knee complications. Causes of Partial ACL Tear A partial ACL tear can result from various injuries or movements that strain the ligament fibers, particularly in sports or high-impact activities. Understanding causes helps in prevention and treatment. Common Causes Include Sudden directional changes: Quick pivoting during sports can overstretch the ACL fibers. Direct impact on the knee: Collisions or falls may partially tear the ligament. Landing awkwardly from jumps: Poor landing technique increases ligament stress and risk of tearing. Overstretching the knee: Excessive bending or twisting beyond normal limits can cause fiber damage. Preventing high-risk movements and strengthening surrounding muscles reduces the likelihood of partial ACL tears. How Partial ACL Tear Diagnosed Diagnosis of a partial ACL tear is essential to distinguish it from a complete rupture and to determine the best treatment approach for optimal recovery. Diagnostic Methods Physical examination tests: Lachman and pivot-shift tests assess ligament stability and knee function. Partial ACL tear MRI: Provides detailed images of ligament fibers to confirm the extent of the tear. X-rays: Help rule out fractures or associated bone injuries. Early and accurate diagnosis ensures proper treatment and reduces the risk of chronic knee instability. Treatment Options for Partial ACL Tear Treatment for a partial ACL tear depends on severity, activity level, and knee stability, with many cases responding well to non-surgical care. Non-Surgical Treatment Rest and activity modification: Limiting strenuous movements helps damaged fibers heal properly. Ice therapy: Reduces swelling and alleviates discomfort in the injured knee. Pain medications: Over-the-counter drugs may help manage moderate knee pain effectively. Knee brace for ACL tear: Stabilizes the knee and prevents additional ligament strain. Physical therapy exercises: Strengthens muscles and improves overall knee function safely. Most partial ACL tears recover successfully without surgery when patients adhere to rehabilitation programs. Surgical Treatment Indicated for unstable knees: Surgery may be required if knee stability is significantly compromised. Associated injuries: Meniscus or cartilage damage often requires operative repair along with ACL reconstruction. Athletes needing full stability: Competitive sports participants may undergo surgery for optimal performance. Surgical treatment is generally reserved for severe partial tears or unstable knees. Recovery After Partial ACL Tear Recovery from a partial ACL tear depends on ligament damage extent, age, overall health, and commitment to rehabilitation exercises. Proper care prevents long-term knee issues. Recovery Factors Include Extent of ligament damage: More fiber tears result in a longer healing period and rehabilitation. Age and health: Younger and healthier patients typically regain strength and mobility faster. Consistency with physiotherapy: Regular exercises improve stability and muscle strength effectively. Activity modification: Avoiding high-impact sports ensures safer ligament healing. Recovery timelines may range from 4 to 12 weeks, with consistent therapy being the key to success. Exercises and Rehabilitation for Partial ACL Tear Rehabilitation exercises are essential for restoring knee strength, stability, and flexibility after a partial ACL tear, reducing the risk of re-injury. Common Exercises Include Range-of-motion exercises: Gradual bending and straightening prevent stiffness and promote healing. Strengthening exercises: Quadriceps, hamstrings, and glute muscles support the knee joint. Balance and coordination drills: Enhance stability and prevent future ligament injuries effectively. Functional exercises: Simulate daily and sports movements to regain full knee function. Structured rehabilitation ensures safer recovery and improves long-term knee health after injury. Long-Term Effects of Partial ACL Tear Without Surgery Ignoring a partial ACL tear can lead to chronic instability, recurrent injuries, and degenerative joint changes over time. Potential Complications Chronic knee instability: The knee may repeatedly “give way,” affecting daily activities. Recurrent injury: Unhealed fibers increase the likelihood of further ligament damage. Early-onset arthritis: Poor healing may accelerate cartilage wear and joint degeneration. Reduced mobility:
Best Treatment Options for Posterior Shoulder Dislocation: From Reduction to Surgery

Best Treatment Options for Posterior Shoulder Dislocation: From Reduction to Surgery Posterior shoulder dislocation is a rare but serious medical condition in which the head of the humerus moves backward out of the shoulder socket. Due to subtle clinical signs, posterior shoulder dislocation is often missed during initial examination, leading to delayed treatment and a higher risk of complications. In many cases, Shoulder Dislocation is incorrectly diagnosed as a simple shoulder strain or frozen shoulder, which can worsen joint stability over time. Unlike anterior shoulder dislocation, posterior shoulder dislocation usually occurs due to seizures, electric shock, high-impact trauma, or forceful internal rotation of the arm. Patients with osterior Shoulder Dislocation commonly experience shoulder pain, stiffness, restricted external rotation, and difficulty lifting the arm. Early diagnosis of posterior shoulder dislocation is essential to prevent joint damage, instability, and the risk of recurrent shoulder dislocation. Understanding Posterior Shoulder Dislocation Posterior shoulder dislocation occurs when the humeral head is displaced backward from the glenoid socket. It usually results from seizures, electrical shock, trauma, or forceful internal rotation of the arm. Because symptoms may appear subtle, posterior shoulder dislocation is frequently misdiagnosed as a simple shoulder injury or muscle strain. Common Symptoms Include: Severe shoulder pain and stiffness Limited external rotation Flattened anterior shoulder appearance Early recognition of posterior shoulder dislocation is critical to prevent recurrent shoulder dislocation and cartilage damage. Types of Shoulder Dislocation Understanding shoulder dislocation types helps determine the correct treatment plan. These include anterior, posterior, and inferior dislocations. Each type differs in cause, symptoms, and severity. Proper identification ensures timely shoulder dislocation treatment, reduces complications, and lowers the risk of recurrent shoulder dislocation and long-term joint instability. Anterior shoulder dislocation (most common) Posterior shoulder dislocation (rare but often missed) Inferior shoulder dislocation (luxatio erecta) Diagnosis of Posterior Shoulder Dislocation Shoulder dislocation types include anterior, posterior, and inferior dislocations. Each varies in cause, symptoms, and severity. Correct identification allows timely shoulder dislocation treatment, helps restore joint stability, and reduces pain, complications, and the risk of recurrent shoulder dislocation. Imaging Techniques Used: Standard X-ray (AP view may appear normal) Axillary view X-ray CT scan for bone defects MRI for soft tissue damage Because posterior shoulder dislocation can be overlooked on routine imaging, advanced scans are often required before deciding on treatment. Non-Surgical Treatment Options 1. Closed Reduction Closed reduction is the first-line treatment for acute posterior shoulder dislocation if diagnosed early. This procedure involves gently guiding the dislocated shoulder back into position under sedation or anesthesia. Key points of closed reduction: Best within 24–48 hours of injury Requires experienced orthopedic handling Followed by immobilization After reduction, the shoulder is immobilized using a brace to allow healing and prevent a dislocated shoulder from recurring. 2. Immobilization and Physiotherapy Once the posterior shoulder dislocation is reduced, immobilization is followed by guided physiotherapy. Rehabilitation focuses on: Restoring shoulder mobility Strengthening rotator cuff muscles Preventing recurrent shoulder dislocation This conservative shoulder dislocation treatment works well in first-time, stable cases without bone defects. When Surgery Is Required Surgery becomes necessary when closed reduction fails, the dislocation is old or recurrent, significant bone damage exists, or shoulder instability continues despite proper rehabilitation and conservative shoulder dislocation treatment. Closed reduction fails The dislocation is old or neglected There is recurrent shoulder dislocation Significant bone or cartilage damage exists Delayed treatment of posterior shoulder dislocation increases the risk of chronic pain and joint instability. Shoulder Dislocation Surgery Options 1. Open Reduction Surgery Open reduction is performed when closed reduction is not possible. The surgeon directly visualizes the joint and repositions the humeral head. This type of shoulder dislocation surgery is usually required in locked posterior shoulder dislocation cases. 2. Bone Defect Reconstruction In chronic posterior shoulder dislocation, bone defects (reverse Hill-Sachs lesions) may be present. Surgical reconstruction helps restore joint stability. Common procedures include: Bone grafting Modified McLaughlin procedure Tendon transfer techniques These procedures significantly reduce the risk of recurrent shoulder dislocation. 3. Arthroscopic Shoulder Surgery Minimally invasive arthroscopy is widely used for posterior shoulder dislocation treatment because it allows precise repair through small incisions. This technique reduces pain, limits tissue damage, improves joint visualization, speeds recovery, and helps restore shoulder stability while lowering the risk of recurrent shoulder dislocation. Benefits include: bility while lowering the risk of recurrent shoulder dislocation. Smaller incisions Faster recovery Less post-operative pain Arthroscopy is ideal for patients with soft tissue injuries and instability rather than major bone loss. Recovery After Posterior Shoulder Dislocation Treatment Recovery depends on whether the posterior shoulder dislocation was treated conservatively or surgically. Typical Recovery Timeline: Immobilization: 3–6 weeks Physiotherapy: 6–12 weeks Full activity: 3–6 months Following shoulder dislocation surgery, rehabilitation is crucial to regain strength and prevent another dislocated shoulder. Preventing Recurrent Shoulder Dislocation To avoid recurrence after posterior shoulder dislocation treatment: Follow physiotherapy strictly Avoid early heavy lifting Strengthen shoulder stabilizers Address seizure disorders if present Proper post-treatment care greatly reduces the chances of recurrent shoulder dislocation and long-term complications. FAQs What is posterior shoulder dislocation? Posterior shoulder dislocation occurs when the upper arm bone moves backward out of the shoulder joint. It is less common than other shoulder dislocation types and is often missed during early diagnosis. What causes posterior shoulder dislocation? Posterior shoulder dislocation is commonly caused by seizures, electric shock, high-impact trauma, or forceful internal rotation of the arm. These events push the shoulder backward, leading to joint instability. How is posterior shoulder dislocation diagnosed? Diagnosis of posterior shoulder dislocation requires special X-ray views, CT scan, or MRI. Standard X-rays may not clearly show the injury, which is why osterior Shoulder Dislocation is sometimes overlooked. What are the treatment options for posterior shoulder dislocation? Treatment depends on severity and timing. Options include closed reduction, immobilization, physiotherapy, and in severe or recurrent cases, shoulder dislocation surgery. Can posterior shoulder dislocation happen again? Yes, posterior shoulder dislocation can recur if not treated properly or if rehabilitation is incomplete. Proper shoulder dislocation treatment and muscle strengthening
What Is Knee Ligament Surgery? Types, Procedure & Recovery

What Is Knee Ligament Surgery? Types, Procedure & Recovery Knee ligament surgery is a specialized orthopedic procedure performed to repair or reconstruct damaged ligaments in the knee joint. Knee ligament injuries are common among athletes, active individuals, and even older adults due to accidents, sports injuries, or degenerative changes. When non-surgical treatment fails, knee ligament surgery becomes essential to restore knee stability, strength, and normal movement. Understanding knee ligaments, their function, types of injuries, and recovery after knee ligament surgery helps patients make informed decisions and achieve better long-term outcomes. What Is Knee Ligament Surgery? Knee ligament surgery is performed to repair or reconstruct torn or severely damaged knee ligaments. In most cases, surgeons reconstruct the ligament using a graft rather than stitching the torn ligament directly. This surgery is commonly recommended when a knee ligament tear leads to: Chronic knee instability Repeated knee giving way Inability to return to sports or daily activities Failure of conservative knee ligament injury treatment Modern knee ligament surgery is usually done using minimally invasive arthroscopic techniques, ensuring faster recovery and reduced pain. What Are Knee Ligaments and Why Are They Important? The knee joint is one of the most complex joints in the human body. It depends heavily on the knee ligaments to maintain stability and proper movement. Knee joint ligaments connect bones to bones and prevent excessive movement that could damage the joint. The four main knee ligaments include: Anterior Cruciate Ligament (ACL) – Controls forward movement of the shin bone Posterior Cruciate Ligament (PCL) – Prevents backward movement of the shin bone Medial Collateral Ligament (MCL) – Provides inner knee stability Lateral Collateral Ligament (LCL) – Stabilizes the outer knee Damage to any of these knee joint ligaments can cause pain, swelling, instability, and difficulty walking or playing sports. Types of Knee Ligament Surgery Different types of knee ligament surgery are performed based on the specific ligament injured. ACL Knee Ligament Surgery ACL reconstruction is the most common knee ligament surgery, especially in athletes. Uses tendon grafts from hamstring, patellar, or donor tissue Restores knee stability during twisting movements Prevents long-term joint damage PCL Knee Ligament Surgery PCL injuries may require surgery when instability persists. Usually performed for severe ligament tears Helps regain knee strength and function MCL Knee Ligament Surgery Most MCL injuries heal without surgery, but surgery is required when: There is a complete knee ligament tear Multiple ligaments are damaged LCL Knee Ligament Surgery LCL injuries often occur with other ligament injuries and require surgical repair for stability. Causes of Knee Ligament Tear A knee ligament tear occurs due to sudden injury or repeated stress on the knee. It is commonly caused by sports activities, sudden twisting movements, direct impact, falls, or accidents, leading to pain, swelling, instability, and difficulty in normal knee movement. Sports injuries (football, cricket, basketball, skiing) Sudden twisting or pivoting movements Direct blow to the knee Road traffic accidents Falls or missteps Degenerative weakening of the knee ligaments Knee Ligament Tear Symptoms Recognizing knee ligament tear symptoms early is important to avoid further damage. Common symptoms include sudden knee pain, swelling, stiffness, instability, difficulty walking, reduced movement, and a popping sensation at the time of injury, especially during sports or sudden twisting activities. Common symptoms include: Sudden knee pain Swelling within hours of injury Knee instability or “giving way” Difficulty walking or running Reduced range of motion Popping sensation at the time of injury Persistent knee ligament tear symptoms often indicate the need for advanced knee ligament injury treatment or surgery. Diagnosis Before Knee Ligament Surgery Accurate diagnosis is crucial before performing knee ligament surgery. Doctors use a combination of: Physical examination X-rays (to rule out fractures) MRI scans (gold standard for knee ligament injuries) MRI helps visualize knee joint ligaments clearly and determine the severity of the tear. Procedure of Knee Ligament Surgery Modern knee ligament surgery is typically performed arthroscopically. Step-by-Step Knee Ligament Surgery Procedure Anesthesia – General or spinal anesthesia is given Arthroscopic Evaluation – Small incisions are made to insert a camera Removal of Torn Ligament – Damaged tissue is cleared Graft Placement – New ligament graft is positioned Fixation – Graft is secured with screws or anchors Closure – Incisions are closed with minimal scarring This minimally invasive approach reduces pain and speeds up recovery after knee ligament surgery. Knee Ligament Injury Treatment: Surgery vs Non-Surgical Care Not every knee injury needs surgery. Knee ligament injury treatment depends on the severity of the tear, knee stability, and the patient’s activity level. Mild injuries often heal with rest and physiotherapy, while severe or unstable ligament tears may require surgical treatment for full recovery. Non-Surgical Treatment Options Rest and activity modification Knee braces Physiotherapy Pain management When Knee Ligament Surgery Is Recommended Complete ligament tear Persistent instability Failure of conservative treatment Athletes want full performance recovery Recovery After Knee Ligament Surgery Recovery plays a vital role in the success of knee ligament surgery. Proper physiotherapy, guided exercises, and gradual activity progression help restore strength, flexibility, and stability of the knee, reduce complications, and ensure a safe return to daily activities and sports over time. Recovery Timeline Week 1–2: Pain control and swelling reduction Weeks 3–6: Regaining knee motion and strength Months 3–6: Advanced strengthening and balance training 6–9 Months: Return to sports activities Physiotherapy After Knee Ligament Surgery Physiotherapy focuses on: Strengthening muscles around the knee Improving balance and coordination Protecting healing knee ligaments Skipping rehab can compromise surgical results. Benefits of Knee Ligament Surgery Successful knee ligament surgery helps restore knee stability, reduce long-term pain, and improve mobility. It allows patients to return to daily activities and sports safely, prevents further joint damage, and enhances overall knee strength and confidence with proper rehabilitation and care. Restores knee stability Reduces chronic pain Prevents further joint damage Improves mobility and confidence Allows safe return to sports and an active lifestyle Risks and Complications of Knee Ligament Surgery Although safe, knee ligament surgery may involve some risks: Infection Stiffness Blood clots
Bad Signs After ACL Surgery: Warning Symptoms You Shouldn’t Ignore

Bad Signs After ACL Surgery: Warning Symptoms You Shouldn’t Ignore ACL surgery is often a turning point for people dealing with serious knee injuries. It promises stability, strength, and a return to normal movement. However, recovery is not always smooth for everyone. While some discomfort is part of healing, certain symptoms may signal deeper problems. These Bad Signs After ACL Surgery should never be ignored because they can affect long-term knee function if left unaddressed. Many patients feel unsure about what is normal after surgery and what is not. This confusion often leads to delays in identifying complications. In this detailed guide, we will break down what to expect after ACL surgery, common warning signs, recovery challenges, and how to understand your body better during healing. Knowing these signs early can protect your knee and support a safer recovery journey. What is ACL surgery and the Recovery Process ACL surgery is performed to repair or reconstruct the anterior cruciate ligament, which is crucial for knee stability. This ligament helps control twisting, pivoting, and sudden movements. Injuries often occur during sports, falls, or accidents. After ACL surgery, the body begins healing in phases. Common experiences include: Swelling around the knee joint Pain or soreness, especially in the first few weeks Stiffness and reduced range of motion Weakness in the thigh muscles These symptoms usually improve gradually with physiotherapy and rest. However, Bad Signs After ACL Surgery appear when recovery stalls or symptoms worsen instead of improving. Recognizing this difference early is essential. Pain After ACL Surgery: When Normal Turns Into a Warning Pain is expected after surgery, but pain after ACL surgery should slowly decrease with time. One of the most common Bad Signs After ACL Surgery is pain that increases instead of settling down. Pain becomes concerning when: It feels sharp, stabbing, or deep inside the knee It worsens at night or disrupts sleep It increases during simple activities like walking It does not improve despite rest and exercises Mild discomfort during physiotherapy is normal. However, constant or worsening pain may interfere with rehabilitation and extend ACL surgery recovery time. Listening to pain signals helps prevent further complications. Swelling That Refuses to Go Away Swelling is a natural response after surgery, but persistent swelling is one of the clear Bad Signs After ACL Surgery. Normal swelling: Reduces gradually over weeks Improves with rest, elevation, and exercise Abnormal swelling may include: Knee remaining visibly swollen for long periods Tight or heavy sensation in the joint Difficulty bending or straightening the knee Warmth around the knee that does not subside When swelling and stiffness occur together, they can restrict movement and slow recovery. Managing swelling early helps prevent long-term joint stiffness. Delayed ACL Surgery Recovery Time and Limited Mobility Regaining knee movement is a major goal after surgery. One of the concerning Bad Signs After ACL Surgery is delayed progress in movement and flexibility. Signs of delayed recovery include: Difficulty fully straightening the knee Limited bending even after weeks of therapy Painful walking or limping No noticeable improvement despite regular physiotherapy A delayed ACL surgery recovery time can affect muscle strength, balance, and confidence. Early attention to limited mobility can prevent permanent restrictions and support better outcomes. Knee Instability and the “Giving Way” Feeling A feeling of instability is one of the most serious Bad Signs After ACL Surgery. The surgery aims to restore knee stability, so ongoing instability is not normal. Warning signs include: Knee buckling during walking Sudden loss of balance Fear of putting weight on the leg Difficulty turning or changing direction This sensation can increase the risk of re-injury and affect daily activities. During early recovery, support tools like a Knee Brace for ACL Injuries can help improve confidence, but persistent instability should always be addressed. Infection-Related Symptoms You Should Watch For Although uncommon, infection-related symptoms are important Bad Signs After ACL Surgery and should not be overlooked. Possible warning signs include: Increasing redness around the incision Unusual fluid discharge Foul smell from the surgical site Persistent warmth or tenderness While mild tenderness is expected, worsening symptoms over time may delay healing and prolong recovery. Paying attention to incision changes is a key part of recovery awareness. Challenges After ACL and Meniscus Surgery Some patients undergo ACL and meniscus surgery together. This combined procedure often requires more careful rehabilitation. Recovery challenges may include: Slower improvement in movement Increased stiffness Joint locking or clicking sensations Uneven pain distribution While a slightly longer recovery is normal, worsening symptoms may become Bad Signs After ACL Surgery if ignored. Understanding these challenges helps patients set realistic expectations and respond early. Emotional and Mental Signs That Affect Recovery Recovery is not just physical. Emotional changes can also be subtle Bad Signs After ACL Surgery. Common emotional challenges include: Fear of re-injury Frustration with slow progress Loss of confidence in knee strength Anxiety about returning to sports or work Mental stress can indirectly slow physical recovery. Staying informed and patient-focused during ACL Injury & Reconstruction Surgery recovery helps maintain motivation and consistency. Exploring Treatment Options and Cost Awareness When recovery does not go as planned, timely adjustments make a big difference. Important considerations include: Physiotherapy modifications Supportive braces or aids Follow-up assessments Understanding acl surgery cost is also important for long-term planning. Costs may vary depending on treatment needs, rehabilitation duration, and follow-up care. Some individuals explore acl tear treatment without surgery for partial tears, but post-surgical symptoms should never be ignored. Early care often reduces long-term expenses and recovery time. Normal Healing vs Bad Signs After ACL Surgery Recovery Aspect Normal Healing Bad Signs After ACL Surgery Pain Gradually decreases Becomes severe or constant Swelling Reduces over time Persists or worsens Movement Improves steadily Remains restricted Stability Knee feels secure The knee gives way Recovery Time On track Delayed progress Long-Term Effects of Ignoring Warning Signs Ignoring Bad Signs After ACL Surgery can lead to: Chronic knee pain Reduced flexibility Muscle weakness Difficulty returning to sports or work Delays in addressing
Shoulder Pain Exercises for Fast Recovery, Flexibility, and Joint Strength

Shoulder Pain Exercises for Fast Recovery, Flexibility, and Joint Strength Shoulder pain can significantly affect daily activities, work performance, and overall quality of life. From difficulty lifting objects to discomfort while sleeping, shoulder problems are increasingly common due to poor posture, repetitive movements, sports injuries, and aging. The good news is that shoulder pain exercises play a crucial role in reducing pain, restoring flexibility, and strengthening the shoulder joint for long-term relief. This comprehensive guide explains shoulder pain causes, effective shoulder pain exercises, treatment approaches, and recovery tips to help you regain pain-free movement safely and efficiently. Understanding Shoulder Pain and Its Impact on Daily Life The shoulder is one of the most mobile joints in the body, making it more vulnerable to injury and strain. Shoulder joint pain can occur suddenly due to trauma or gradually due to overuse and degeneration. Common symptoms include: Pain during arm movement Stiffness or reduced range of motion Weakness in the arm Pain radiating to the neck or upper arm Difficulty performing overhead activities Conditions such as left side shoulder pain, left hand shoulder pain, and chronic shoulder pain often worsen when ignored or treated incorrectly. Causes of Shoulder Pain You Should Not Ignore Understanding the causes of shoulder pain is essential before starting shoulder pain exercises because different conditions require different treatment approaches. Shoulder pain may result from muscle strain, ligament injury, joint degeneration, or nerve-related issues. Identifying the exact cause helps in selecting the right exercises, avoiding movements that may worsen the condition, and ensuring faster, safer recovery. Without proper diagnosis, incorrect exercises can increase inflammation, prolong pain, or lead to chronic shoulder problems. Shoulder Pain Causes Related to Injury Rotator cuff tears Shoulder dislocation Sports-related injuries Falls or accidents Overuse injuries Medical and Lifestyle-Related Causes of Shoulder Pain Frozen shoulder Arthritis Tendinitis or bursitis Poor posture Repetitive strain Both left-sided shoulder pain and shoulder injury pain can develop due to improper movement patterns and lack of shoulder strength. Why Shoulder Pain Exercises Are Essential for Recovery Shoulder pain exercises are a cornerstone of non-surgical treatment and rehabilitation. When performed correctly, these exercises help: Reduce inflammation and stiffness Improve flexibility and joint mobility Strengthen shoulder muscles Enhance blood circulation Prevent recurrence of shoulder pain Unlike medication that offers temporary relief, shoulder pain exercises address the root cause of pain and promote long-term healing. When to Start Shoulder Pain Exercises You can begin shoulder pain exercises when: Acute pain and swelling have reduced A doctor or physiotherapist confirms it is safe Pain does not worsen with gentle movement For chronic shoulder pain, exercises are often introduced gradually and adjusted based on pain tolerance. Best Shoulder Pain Exercises for Flexibility and Mobility 1. Pendulum Exercise for Shoulder Pain Relief This is one of the safest shoulder pain exercises, especially during early recovery. How to perform: Bend forward slightly, letting the affected arm hang down Gently swing the arm in small circles Perform clockwise and counterclockwise movements Benefits: Relieves stiffness Improves joint lubrication Reduces shoulder joint pain 2. Cross-Body Shoulder Stretch Helpful for left hand shoulder pain. How to perform: Bring the affected arm across your chest Use the opposite hand to gently pull it closer Hold for 20–30 seconds Benefits: Improves flexibility Reduces muscle tightness Enhances shoulder pain relief Strengthening Shoulder Pain Exercises for Joint Stability 1. Wall Push-Ups One of the safest strengthening shoulder pain exercises. How to perform: Stand facing a wall Place your hands on the wall at shoulder height Slowly bend your elbows and push back Benefits: Builds shoulder stability Strengthens surrounding muscles Supports shoulder pain treatment 2. Resistance Band External Rotation Ideal for rotator cuff strengthening and shoulder injury pain recovery. How to perform: Hold a resistance band with your elbow bent at 90 degrees Rotate the arm outward slowly Repeat 10–15 times Benefits: Improves shoulder joint strength Prevents future injuries Supports long-term recovery Advanced Shoulder Pain Exercises for Chronic Conditions For individuals suffering from Shoulder Ligament Injury, advanced exercises should be performed under professional supervision. 1. Shoulder Blade Squeeze This exercise targets posture-related shoulder pain causes. How to perform: Sit or stand upright Squeeze shoulder blades together Hold for 5 seconds Benefits: Improves posture Reduces muscle imbalance Decreases shoulder joint pain 2. Overhead Arm Stretch Effective for stiffness and frozen shoulder. How to perform: Raise the affected arm overhead Use the other hand to assist gently Hold for 15–20 seconds Benefits: Enhances flexibility Reduces movement-related pain Improves range of motion Role of Shoulder Pain Exercises in Shoulder Pain Treatment Modern shoulder pain treatment emphasizes conservative care before surgery. Shoulder pain exercises are often combined with: Physiotherapy Heat or cold therapy Pain management techniques Posture correction Activity modification This holistic approach ensures safe and sustainable recovery. Tips to Maximize Results from Shoulder Pain Exercises To get the best outcomes from shoulder pain exercises, follow these guidelines: Perform exercises slowly and with control Avoid movements that increase pain Maintain proper posture Be consistent with your routine Combine exercises with rest and recovery Ignoring pain signals can worsen shoulder injury pain and delay healing. Preventing Shoulder Pain with Regular Exercises Prevention is as important as treatment. Regular shoulder pain exercises help: Strengthen shoulder muscles Improve joint stability Prevent recurring injuries Reduce the risk of chronic shoulder pain People with desk jobs, athletes, and older adults benefit greatly from preventive shoulder exercises. When to Seek Medical Help for Shoulder Pain Consult a specialist if: Pain persists for more than two weeks Movement becomes severely restricted Pain radiates down the arm You experience weakness or numbness Professional guidance ensures the safe progression of shoulder pain exercises and effective treatment. FAQs Are shoulder pain exercises safe for everyone? Yes, shoulder pain exercises are generally safe when performed correctly. However, individuals with severe pain, recent injury, or surgery should consult a specialist before starting. How often should I do shoulder pain exercises? Most shoulder pain exercises can be done 1–2 times daily. Consistency is more important than intensity for
Knock Knees Exercises to Reduce Pain and Correct Knee Position

Knock Knees Exercises to Reduce Pain and Correct Knee Position If you are struggling with misaligned knees, performing the right Knock Knees Exercises can significantly help you in reducing pain, improving alignment, and preventing long-term complications. Knock knees, medically referred to as genu valgum, is a problem that affects children, teenagers, and adults. Left untreated, misaligned knees can place extra stress on your joints and even contribute to a knee ligament injury. This blog will guide you through effective exercises, assessments, and treatment options to naturally correct knock knees and protect your knee health. This comprehensive guide will help you understand how to check knock knees, explore effective exercises, and provide insights into knock knees treatment, including braces and surgical options when necessary. What Are Knock Knees? Knock knees occur when the knees angle inward and touch each other while the ankles remain apart. This can affect your posture, walking gait, and overall leg alignment. In adults, knock knees are often associated with weak hip muscles, improper posture, or obesity, whereas in children, they may be a normal stage of growth. Key indicators of knock knees include: Knees that touch while standing upright Ankles that remain apart Uneven gait or difficulty walking Knee, hip, or lower back discomfort Untreated knock knees may lead to early knee arthritis or chronic pain. That’s why early knock knees treatment and corrective exercises are vital for long-term knee health. How to Check Knock Knees at Home Understanding how to check knock knees at home is simple but important. A home assessment can help determine if a professional evaluation is needed. Steps to Check: Stand upright with your back against a wall Place your knees together naturally Measure the gap between your ankles If the ankle gap exceeds 5–6 cm, it may indicate knock knees. However, a professional orthopedic assessment is recommended for accurate diagnosis. Early detection allows for effective ways to fix knock knees, including exercises and braces. Causes of Knock Knee Problem The root cause of knock knee problem determines the treatment approach. Common causes include: Muscle weakness: Particularly in the hips and thighs Postural issues: Poor walking or sitting habits Nutritional deficiencies: Lack of calcium or vitamin D Obesity: Extra load on knee joints Injury or arthritis: Past trauma or joint degeneration Genetic factors: Family history of knee deformities Identifying the underlying cause helps target knock knees treatment, whether through exercises, lifestyle adjustments, or surgery. Is Knock Knee Curable? Many people ask, is knock knee curable? The answer depends on the severity and age. Children: Mild cases often self-correct with growth. Adults: Muscle-strengthening exercises can improve alignment, reduce pain, and prevent worsening, though structural correction may require medical intervention. In some severe cases, knock knee surgery may be recommended, but most individuals benefit significantly from consistent Knock Knees Exercises and supportive treatments. Role of Knock Knees Exercises in Correction Knock Knees Exercises are essential because they: Strengthen weak muscles (glutes, hips, thighs) Stretch tight inner thighs and calves Improve knee tracking during movement Reduce uneven stress on joints A consistent exercise routine improves knee replacement surgery recovery time and can help prevent future joint problems. Exercises should be performed mindfully and with proper form for maximum benefit. Best Knock Knees Exercises Here are the most effective Knock Knees Exercises for improving alignment and reducing discomfort:a 1. Side-Lying Leg Raises Lie on your side, lift the top leg upward Strengthens outer thighs and hip muscles Helps prevent knees from collapsing inward 2. Clamshell Exercise Lie on your side with knees bent Open your top knee like a clamshell Strengthens glutes and stabilizes the hip 3. Wall Squats with Ball Place a small ball between your knees and squat Builds quadriceps and encourages proper knee tracking Reduces inward knee stress 4. Resistance Band Walks Place a band around your thighs and take sideways steps Improves hip stability and balance Helps fix inward knee motion during walking 5. Inner Thigh Stretch Sit or stand and stretch the inner thigh muscles gently Reduces tension pulling knees inward Essential for posture and alignment Perform these exercises 4–5 times per week. Begin with 10 to 15 reps, and slowly raise the intensity as your strength and comfort improve. How to Fix Knock Knees Naturally To learn how to fix knock knees naturally: Perform daily Knock Knees Exercises Maintain proper posture while walking or sitting Avoid crossing legs for long periods Maintain a healthy body weight Use supportive footwear These simple lifestyle modifications, combined with exercises, often provide significant improvement over time, reducing the need for invasive knock knee surgery. Knee Brace for Knock Knees A knee brace for knock knees can help: Support proper alignment Reduce knee pain during daily activities Increase confidence during exercise While braces do not replace the benefits of strengthening exercises, they are excellent adjuncts, especially in adults or during early rehabilitation after surgery. Knock Knees Treatment Options Knock knees treatment varies based on age, severity, and cause: Non-surgical: Exercises, physical therapy, lifestyle modifications Surgical: Realignment procedures in severe adult cases Supportive devices: Knee braces or orthotic inserts Combining these treatments ensures optimal correction and functional improvement. Informative Table: Exercises and Benefits Exercise Name Primary Benefit Target Area Side Leg Raise Improves alignment Outer thighs Clamshell Reduces knee collapse Glutes Wall Squat with Ball Knee stability Quadriceps Band Walk Hip control Hip abductors Inner Thigh Stretch Reduces inward pull Adductors This table helps visualize how exercises contribute to correcting knock knees effectively. When Knock Knee Surgery May Be Needed Knock knee surgery is considered if: Deformity is severe or painful Non-surgical methods fail Joint damage or arthritis is present Daily activities are significantly impaired Surgery usually involves realigning the bone to restore proper knee mechanics. Post-surgery recovery also benefits from Knock Knees Exercises for long-term stability. Lifestyle Tips to Support Correction Proper nutrition plays a vital role in supporting knee health and enhancing the results of Knock Knees Exercises. Including knee ligament injury recovery food in your diet helps







